Student startup venture takes second place at ACC InVenture competition
The University of North Carolina at Chapel Hill undergrad Sasha Surkin took home second place at this year’s ACC InVenture Prize competition for her startup company WeyeZE, outperforming 12 other ACC teams for the

 | UNC-CH
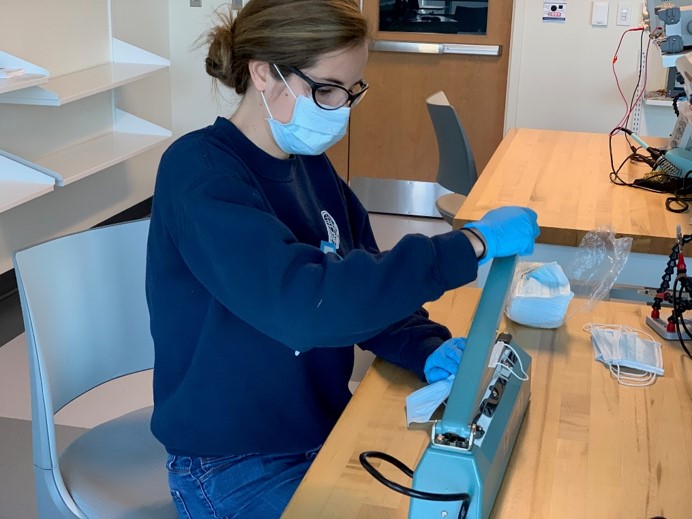
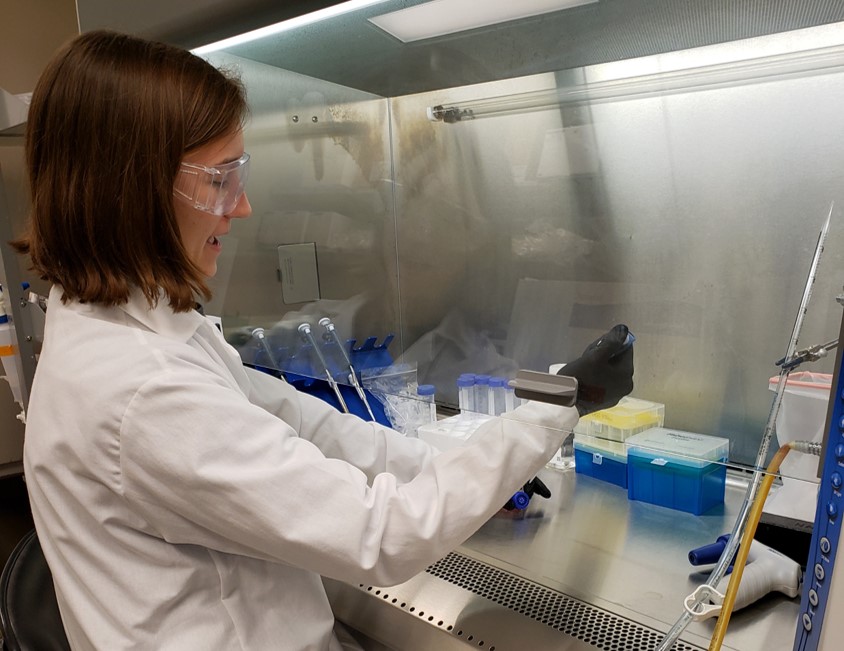
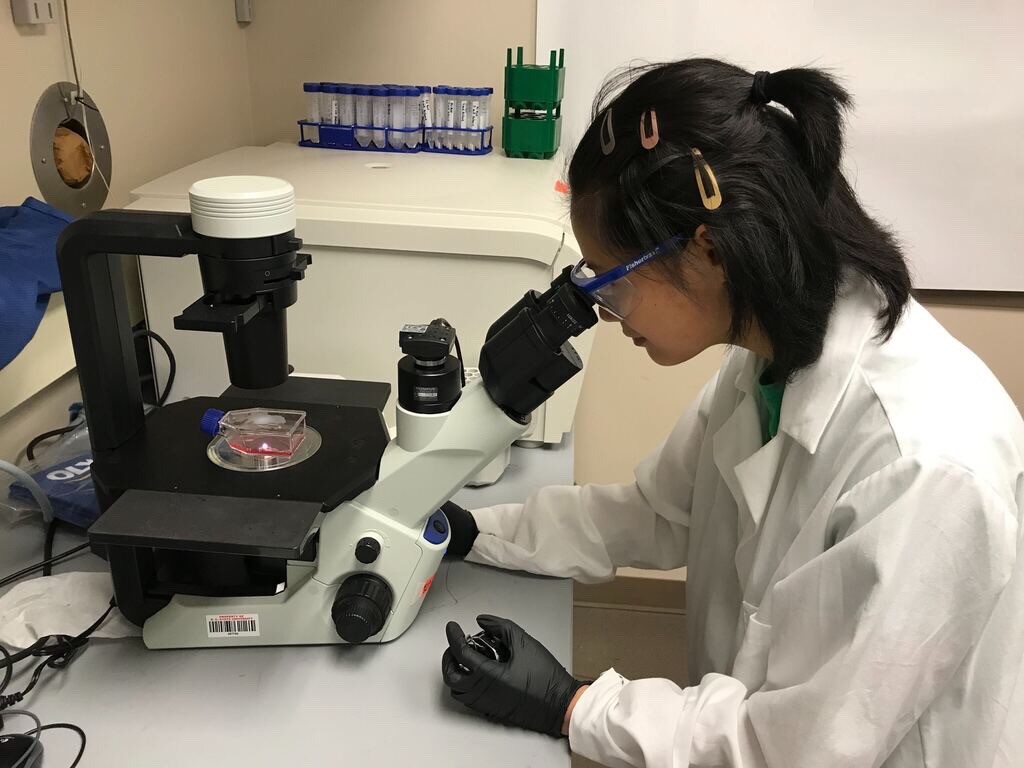
| UNC-CH